It is important for you to get yourself regularly screened for glaucoma.
If you have been diagnosed to have glaucoma, effective treatment options are now available and regular treatment and follow up can help you to preserve your vision for your lifetime, avoiding unnecessary fear of going blind.
You can live happily with glaucoma and enjoy an excellent quality of life, particularly if the disease is detected early and treated in time. Always remember that once you have glaucoma, you will have to be under the care of an eye doctor for the rest of your life.
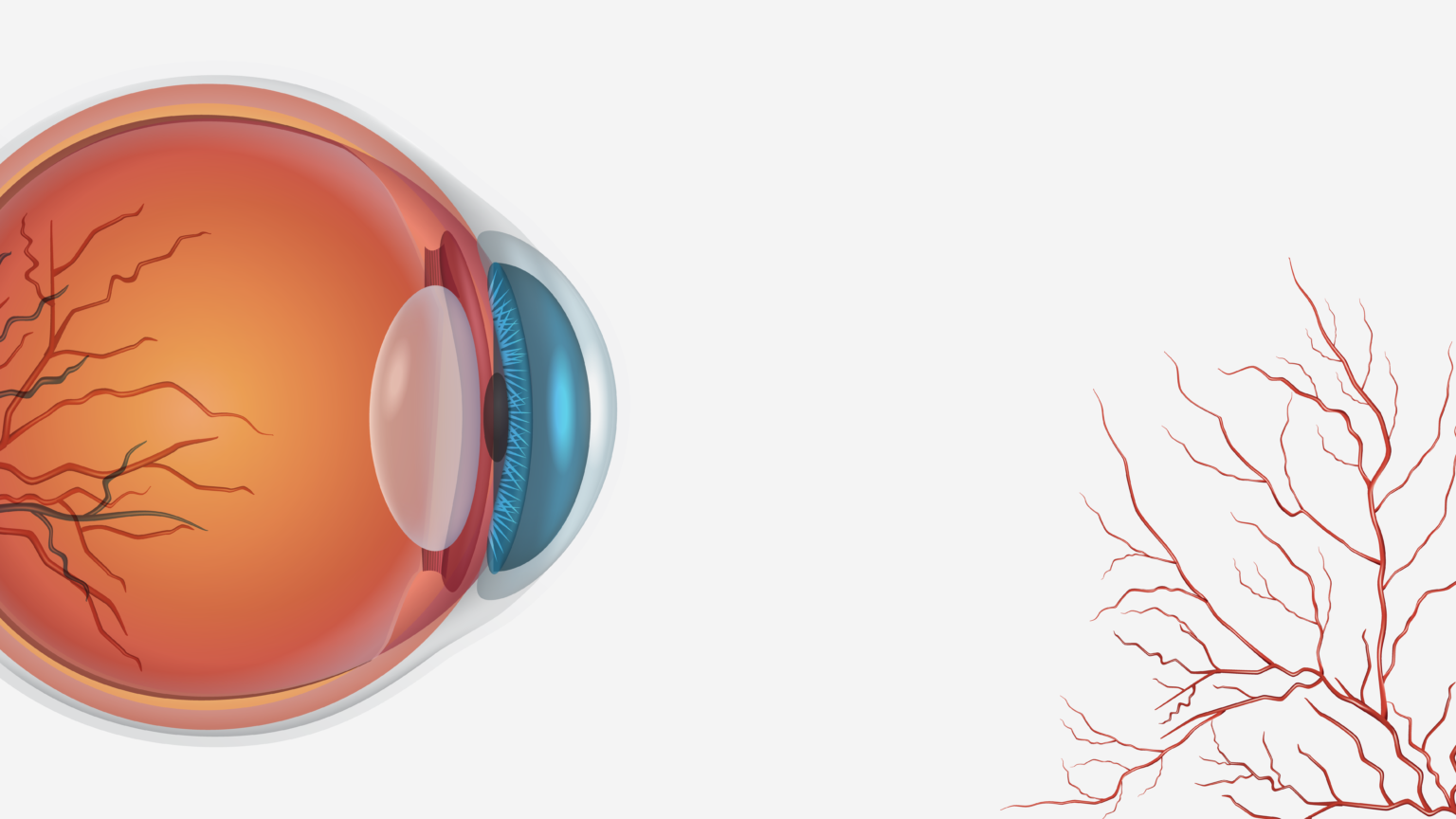
Glaucoma is a disease of the optic nerve of the eye, which is basically the structure that relays what the eye sees to the brain. The major risk factor is represented by the intraocular pressure (IOP). When elevated high, above normal will damage the optic nerve. If left untreated, continued damage to this structure may lead to visual field defects, visual impairment and blindness.
The eye contains a fluid known as aqueous humor that provides nourishment to its internal structures. This fluid is produced behind the iris (colored portion of the eye) and then is drained out through a sieve-like structure called the trabecular meshwork at the front part of the eye. In some eyes, abnormalities in the drainage system leads to impairment of ocular inside fluid outflow, and IOP increases. This high IOP may damage the optic nerve head located in the back part of the eye responsible for the vision. This condition is known as glaucoma. In other cases, IOP may be relatively normal, but glaucoma occurs due to inability of the eye to handle that normal mechanical stress, or because of poor blood supply to these same nerve fibers.
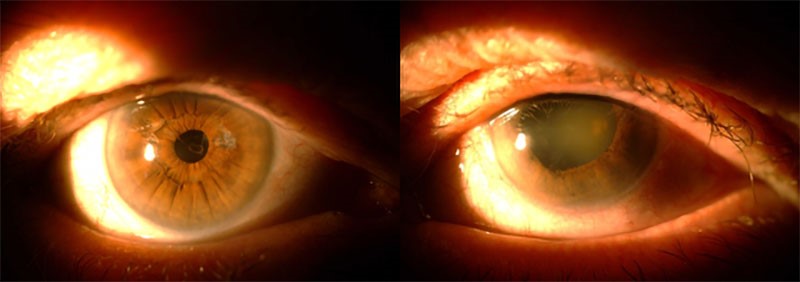
In glaucoma, the optic nerve gets damaged. A portion of the optic nerve may be assessed during the eye exam, where it can be seen as a round structure (optic disc), with the pink or reddish section representing the neural tissue that takes the visual information to the brain. The whitish central part represents absence of neural tissue, and it is called the “cup”. Some amount of cupping is normal, but excessive cupping, or an increase in the amount of cupping over time, suggests glaucoma. There are many blood vessels that emerge from the optic disc to the retina.
Glaucoma causes loss of the neural reddish tissue and there is progressive cupping of the optic disc – enlargement of the whitish central part.
The great majority of glaucoma cases evolve silently, as patients may not notice vision loss until it is significant and present in both eyes, or may assume that vision loss is correctable, as it is for other conditions such as cataract. When the disease is at advanced stages, most patients will then perceive visual abnormalities. Glaucomatous damage to the optic nerve is irreversible, so what is lost cannot be recovered.
The asymptomatic early stages of disease and irreversible nature of the glaucoma makes it one of the main causes of blindness worldwide. Glaucoma does not have a cure, however, this disease can be treated and the worsening of glaucomatous damage can be limited or even stopped. Thus, an early detection associated to an appropriate treatment and follow-up can preserve your vision throughout your lifetime.
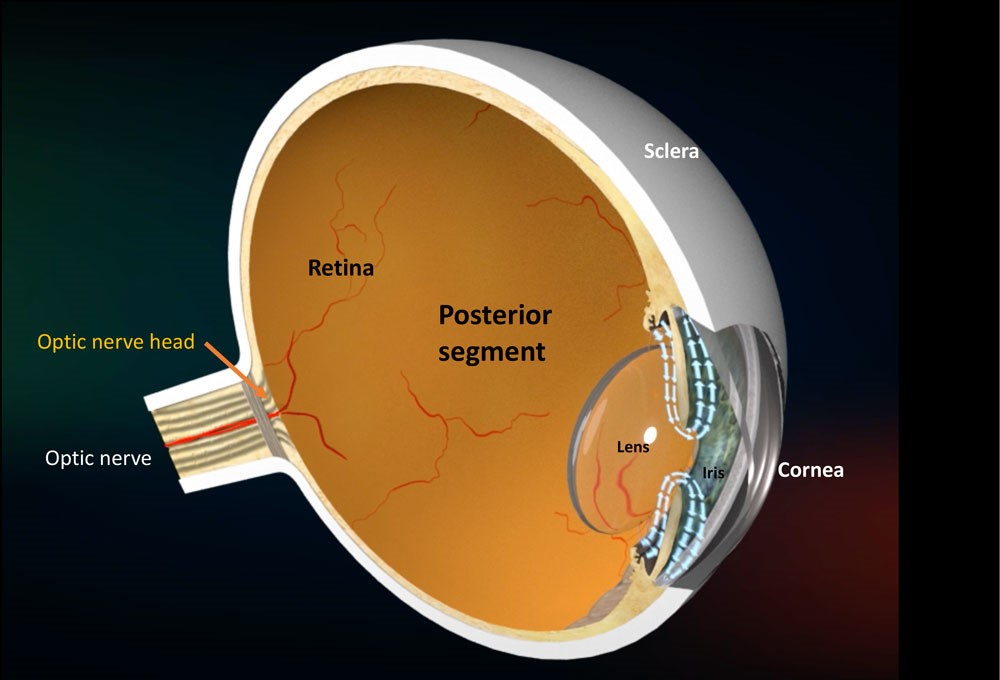
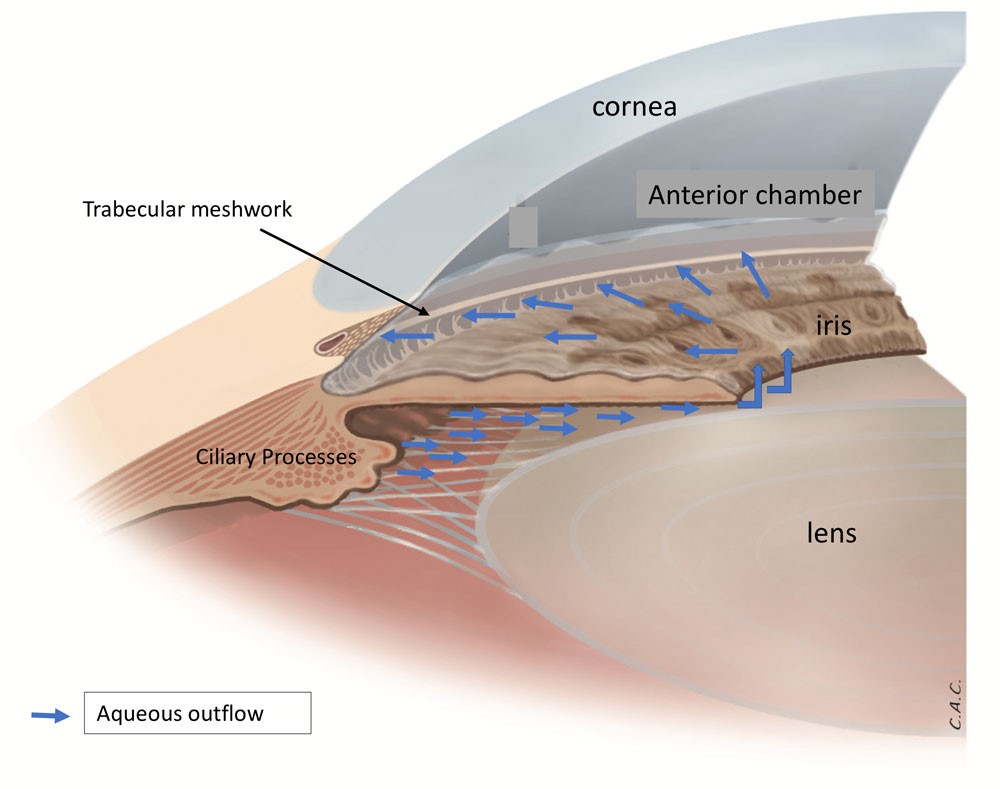
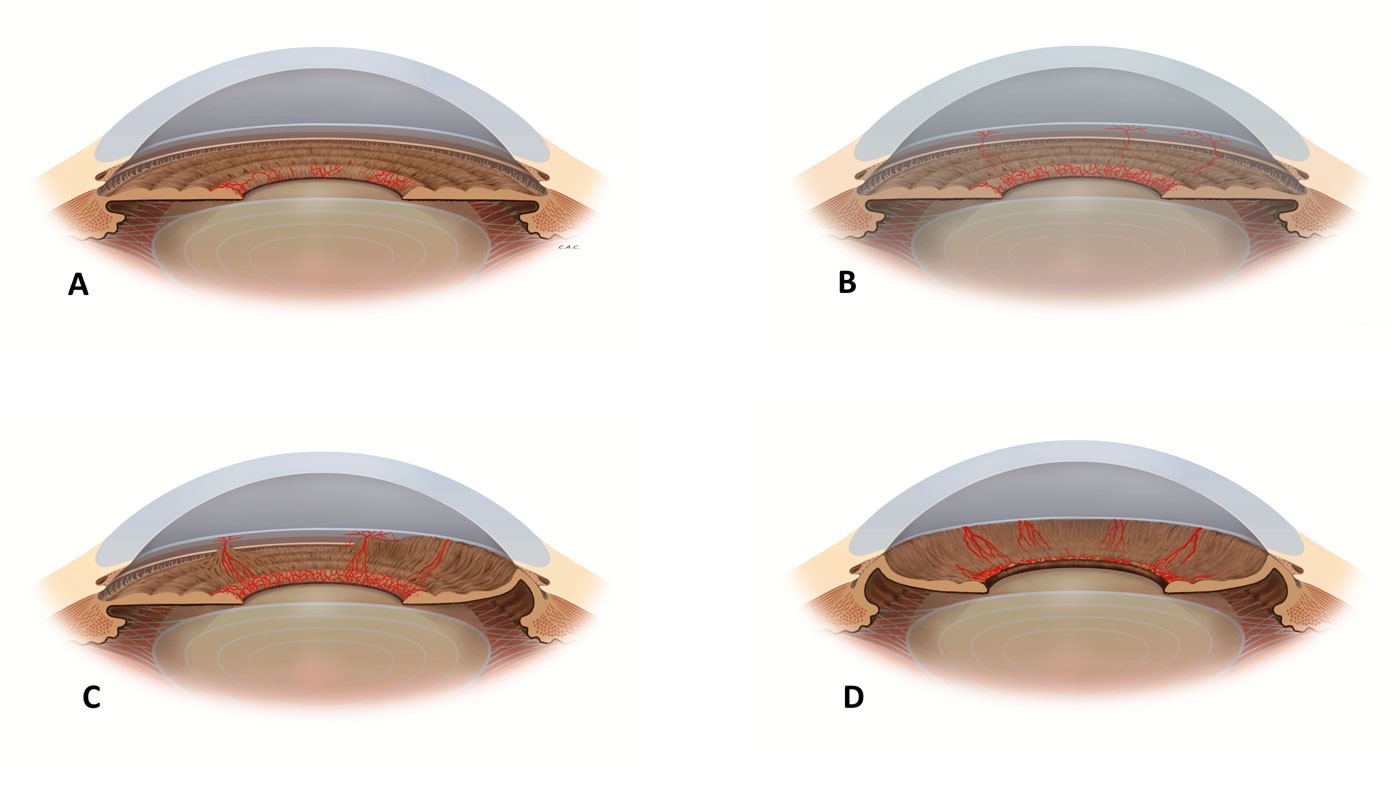
The eye contains a fluid known as aqueous humor that provides nourishment to its structures. This fluid is produced by the ciliary body (located behind the iris) and then flows between the iris and lens, through the pupil to the anterior part of the iris where is drained out through a sieve like structure called the trabecular meshwork, at the anterior chamber angle (located at the merging of the cornea-sclera with the iris periphery).
Many (but not all) cases of glaucoma occur due to a sufficiently elevated IOP, caused by impairment of the normal aqueous humor drainage.
Glaucoma may be classified according to different aspects. Mainly:
Glaucoma is known as the “silent thief of vision” and is typically associated with painless and progressive loss of vision that may not produce any symptoms. Usually, peripheral vision is affected with relative sparing of central vision at early stages of disease, and when the disease gets to advanced stages, the central vision is more severely affected. Glaucoma patients may notice that they cannot see objects at their side (due to loss of peripheral visual field), but largely the patients are not able to detect any symptoms until a very advanced stage. Sometimes, patients may notice or describe that their vision has become foggy (see How does glaucoma evolve?).
Angle-closure glaucoma may be associated with redness, pain in the eye, headache, blurred vision and coloured haloes around light bulbs – acute angle closure attack presenting with quite high IOP levels (above 40 mmHg). However, most angle closure glaucoma cases evolve asymptomatically, as the clogging of the drain and IOP rise tend to occur in a slowly progressive way (see Angle closure glaucoma).
Non-specific vision symptoms may also be associated with glaucoma, like cloudy/foggy vision, glare, or needing more light to read
Glaucoma may occur in babies due to abnormal development of the internal drainage system of the eye. Its signs and symptoms are usually different than adult glaucoma. Classical cases present with enlarged eyes, with a whitish-bluish cloudy appearance as the cornea becomes edematous due to the high IOP. The baby will present intense photophobia (intolerance to light), blepharospasm (i.e. keep eyes shut when exposed to sunlight), and excessive tearing (which may be present in other abnormalities such as nasolacrimal duct obstruction).
Congenital glaucoma is a sight-threatening disease, and a consultation with a glaucoma specialist should be arranged as soon as possible. Examination under anesthesia is required for appropriate assessment of the condition, and treatment is primarily surgical. Early diagnosis and proper treatment are important for a good visual prognosis.
Long-term follow-up is necessary, when the IOP and optic nerve will be monitored, but also, glasses and eye-patching might be necessary for the development and maintenance of a good vision
Normally, glaucoma affects individuals after 40-50 years of age, but it may occur in younger ages. Juvenile glaucoma affects teenagers or young adults and its signs and symptoms are very similar to adult glaucoma. However, juvenile glaucoma may be considered more visual threatening as IOP levels tend to be higher and also, as the disease onset is early in life, there is a need to preserve the optic nerve for a much longer period of time. Therefore, although it is not a common disease, all individuals attending an ophthalmological check up should undergo IOP measurement and optic disc evaluation.

As in all forms of glaucoma, the end-organ damage is the optic nerve head. A sufficiently elevated IOP will damage the optic nerve, which is the structure that connects what the eyes see to the brain.
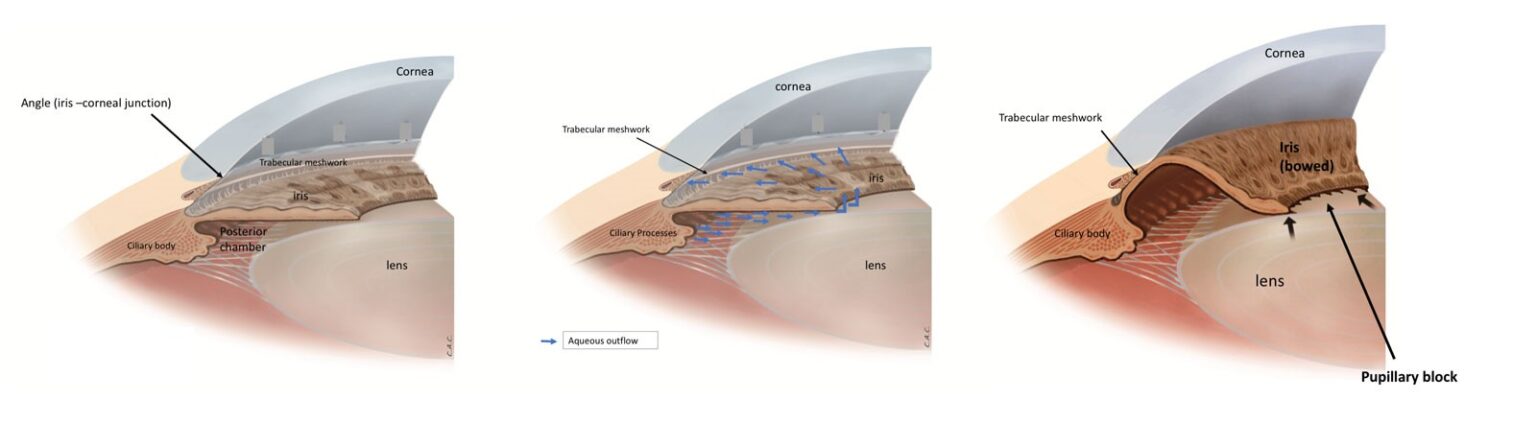
The “angle” is the part of the eye where the iris meets the cornea and the sclera. The drainage system of the eye is located at this region – trabecular meshwork, which consists of multiple layers of collagenous connective tissue. The trabecular beams form a net like structure that creates layers with large and small spaces within the beams.
The open angle glaucoma, as the term suggests, is characterized by an open angle. Nothing obstructs the flow of the aqueous humor to get to the trabecular meshwork, however, abnormalities within the spaces of the trabecular meshwork system lead to increase of the resistance to flow of fluid. The fluid pressure within the eye (IOP) gets elevated, and usually without any symptoms, gradually damages the optic nerve.
his condition occurs in eyes with elevated IOP, without optic nerve damage. Due to individual characteristics that determine a decreased susceptibility to the disease, these eyes do not develop glaucoma. This may be partially explained in some cases due to an increased central corneal thickness (thick cornea), which may lead to imprecise measurement of the IOP by tonometer devices (overestimation of the IOP).
However, it is important to note that some eyes with elevated IOP may be simply at the beginning of the disease process, whereas there was not enough time to damage the optic nerve head. If this is the case, with time, glaucoma will develop.
The ophthalmologist will discuss with the patient the advantages and disadvantages of different management approaches for this condition in each case, including observation only or treatment.
In all Ocular Hypertension cases, continuous long-term follow-up are highly recommended, and some eye exams will be necessary for proper monitoring
Glaucoma suspect is the term used for individuals in which glaucoma diagnosis cannot be confirmed but also cannot be excluded at the time of consultation. In these cases, a mid- or long-term follow-up associated with proper evaluation may be necessary to unveil the presence of disease.
Although this may be considered an uncomfortable situation, it is important to emphasize for the patient to remain calm, as the inability to establish the diagnosis usually occurs in early glaucoma cases and not in advanced cases in which the alterations are more evident.
The inability to confirm the diagnosis may be due to different causes.
The normal appearance of the optic nerve head shows wide variation in the normal population. And in some cases, it may be difficult to differentiate an early glaucomatous optic disc from an optic disc with an unusual appearance (but with no disease).
All individuals diagnosed as glaucoma suspects or with a positive family history of glaucoma should ideally perform proper documentation of the optic disc appearance and visual function status. These exams should be repeated periodically, in order to compare them for changes along mid and long-term follow-up. Along with other exams, determining the presence of deterioration of these variables with time will confirm (or not) the presence of disease.
The ophthalmologist will discuss with the patient the advantages and disadvantages of different management approaches for this condition. In all cases continuous long-term follow-up is highly recommended, and some eye exams are necessary for proper monitoring.
As in all forms of glaucoma, the end-organ damage is the optic nerve head. A sufficiently elevated IOP will damage the optic nerve, which is the structure that connects what the eyes see to the brain.
The “angle” is the part of the eye where the iris meets the cornea and the sclera. The drainage system of the eye is located at this region – trabecular meshwork. (See Open angle glaucoma.)
In primary angle closure glaucoma, the part of the angle where the trabecular meshwork is located is closed/obstructed by the peripheral iris. This angle closure leads to IOP rise and damage to the optic nerve. Angle closure glaucoma usually affects anatomically “small eyes” – in which intra-ocular structures within a limited space area results in a crowded anterior segment
It typically affects more women than men, and although it may occur in any individual, it is more common in some ethnic groups (i.e. Chinese). Most of the cases are asymptomatic, but some show quite intense symptoms. (See Acute angle closure.)
The most common mechanism of angle closure is called pupillary block, and it occurs due to relative block of fluid flow at the level of the pupil (from the posterior to anterior part of the eye), which makes the pressure at the posterior chamber to increase, leading to a forward bowing of the iris and narrowing of the angle
Differentiation between an open angle and a closed angle glaucoma is important because the treatment approach differs, as we may use additional procedures to treat angle closure glaucoma when compared to open angle glaucoma cases.
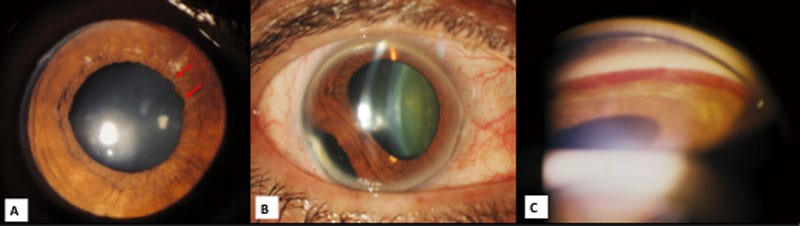
There is a form of angle closure that is very aggressive and shows intense symptoms. In this condition, there is a sudden rise in pressure leading to severe eye pain (and around the eye), redness, decrease in vision. This is known as an acute attack of angle closure and represents a medical emergency, which, if not treated in time, can cause optic nerve damage and loss of vision.
Acute attack symptoms normally occur in one eye, but it may be present in both eyes at the same time. The duration of the symptoms is relatively long (hours), when both pain and decrease vision are often associated. The pupil is often mid-dilated, and the pupil reflex is unresponsive to light.
Episodes of isolated eye pain or isolated blurred vision (minutes) that resolve spontaneously are likely not an acute angle closure attack.
Treatment may include topical and systemic drugs to lower IOP, followed by laser treatment aimed to open the angle (See Laser peripheral iridotomy). In some cases, surgical procedures may also be used to treat this condition.
This is an aggressive form of secondary angle closure glaucoma. It usually affects individuals with retinal disease, mainly retinal vascular occlusion or uncontrolled diabetic retinopathy. The primary abnormality is represented by the retinal ischemia, which releases angiogenic factors. These factors create new vessels at the anterior chamber, usually at the iris pupillary border and the angle wall. These new vessels are abnormal and fragile and will cause a series of events which will lead to secondary angle closure (drainage system obstruction).
The treatment strategy should aim at the primary abnormality (retinal ischemia) and also at the IOP control. This relatively complex form of glaucoma often requires the combined efforts of glaucoma and retina specialists. Diabetic patients should try to maintain as good control of their disease as possible.
Yes, glaucoma can be caused by several medications taken for other diseases, such as Parkinson, epilepsy, depression, allergies, prostate disorders, etc. These represent secondary glaucoma cases.
Particular attention should be given to corticosteroids. Steroid induced glaucoma is a type of glaucoma which develops with the use of medicines known as corticosteroids. It is most commonly noticed with steroid eye drops taken for allergic conjunctivitis/uveitis but can occur with use of steroid containing inhalers (taken by patients who suffer from asthma), nasal spray, skin ointments and any oral or IV medication containing steroids. Moreover, not only corticosteroids may cause glaucoma, but it may also lead to loss of IOP control in patients in treatment for glaucoma.
Thus steroids should be used cautiously and the patients who are using any form of steroid therapy must consult their ophthalmologist (eye specialist) and have their IOP checked regularly.
Of note, particularly for angle closure glaucoma, there are many medications that may trigger or contribute to the angle closure process. Drugs used for depression, migraine, urine incontinence, gastrointestinal disorders and other health conditions can worsen or cause a closed angle. Thus, patients with this form of the disease or suspect of having it should always mention it to their physicians, who will be able to evaluate which medications are safe or not. Also, patients with untreated angle closure or “occludable angles” should be careful when using some medications, even over the counter medications.
When an eye sustains an injury there can be an acute increase in IOP due to damage to the angle structures, hyphema (blood in anterior chamber), inflammation, and other mechanisms. The more severe the trauma, the greater are the chances to develop glaucoma and other ocular complications. But IOP increase may also occur later in life due to damage of the trabecular meshwork. This form of glaucoma can occur even up to 10-20 years after injury. These are also considered secondary glaucoma cases.
It is recommended that any person who has sustained an injury to the eye should get him/herself evaluated for glaucoma, and maintain regular follow-up with an ophthalmologist.
Glaucoma is diagnosed by performing the following 4 essential tests:
In addition to these basic exams, additional tests that may be performed include:
If you have been diagnosed with glaucoma you will require a 3-12 monthly follow-up, depending on the severity of disease, the IOP levels under treatment, and other risk factors. The more severe the disease, the more frequent the follow-up. On the other hand, once the disease is well under control and there are no signs of progression, follow-up at longer intervals may suffice
The bottom line is that the recommended interval between consultations may vary, and should be determined by your ophthalmologist. Of note, glaucoma patients will need follow-up visits for the entire life.
After the initial diagnosis, you will have to get the visual field test repeated to get a good baseline and then repeated more frequently in case the disease is advanced or if your pressure is not under adequate control.
After initial diagnosis, all individuals with glaucoma should perform proper documentation of the optic disc appearance and visual function status. Visual field tests often need to be repeated to get a good and consistent baseline. These exams should then be repeated periodically, in order to compare them for changes along mid and long-term follow-up.
No. Unfortunately glaucoma medicines, laser or surgery cannot improve your vision but can prevent you from further visual loss.
Glaucoma treatment aims to control the intra-ocular pressure and halt glaucoma progression. It is important to understand that glaucoma cannot be cured and whatever damage has occurred to the optic nerve cannot be reversed. However, it is possible to maintain current vision (central and peripheral), so the patient will not develop further visual damage.
Various modalities of treatment are available today. These include:
Eyedrops are usually prescribed as the first line therapy for most types of glaucoma. It is essential to understand that glaucoma does not have a cure, so these drops should be taken on a regular basis, everyday, for your entire life. One of the most important factors in using eye drops for glaucoma is regularity over a long period of time. Consistent/Repetitive failure to comply with eyedrop treatment may result in poor glaucoma control and vision loss.
As a suggestion, you may plan out a schedule for taking your drops around your normal routine, such as when you wake up, brush your teeth, eat meals or when you go to bed at night. You may also set reminders in your cell phone. As a suggestion, after taking a dose, you can put a mark on the calendar so that you remember that you have taken the medicine.
Aim to put only one drop at a time, but if you are not sure the drop got into the eye, you may put an extra drop right away. To optimize eyedrop use, please check What is the correct way of instilling the eyedrops?.
It is recommended to keep a stock of your medication at home, and do not forget to take your eyedrops bottles with you while travelling. Before you visit your eye doctor for check up, always use your eyedrops as usual.
Eyedrops are medicines, and it may be contra-indicated in the presence of some other systemic/ocular diseases. Please remember to tell your doctor if you suffer from any other medical illness like asthma, arrhythmia, bradycardia, diabetes, hypertension, thyroid diseases, angina, arthritis, depression etc., or are taking oral medicines or inhalers for any other condition. The ophthalmologist is able to choose the best treatment strategy for each individual case.
One of the most important factors in using eye drops for glaucoma is regularity over a long period of time. Forgetting to put your eye drops may happen once in a while, but consistent/repetitive failure to comply with eye drop treatment may result in poor glaucoma control and vision loss
If you forget to take a dose of your eye drops, it is best to instill the drop as soon as you remember it. If the next dose is due shortly, wait for the usual time to use it.
Laser is the treatment of choice for angle closure glaucoma and other types of laser may also be performed for open angle glaucoma. Lasers can be performed as an outpatient procedure in a few minutes and may be used to reduce the IOP.
The following types of laser procedures are generally used in glaucoma:
The failure of medications and laser surgery to control the intraocular pressure (IOP) and consequently glaucomatous neuropathy, is an indication for surgery. Surgery may also be performed if the patient has allergy to the drugs, is not compliant to therapy or the disease continues to progress despite treatment. Advanced disease and other conditions are also indication for surgery and the ophthalmologist will discuss the best possible treatment options with the patient.
Can stem cell transplant be done to repair the damaged optic nerve in glaucoma? This is an area of experimental research and until now this treatment is not possible/available for glaucoma patients. However, there are several research groups working on this topic at this moment.
If one has glaucoma, are there any changes in life-style which can help to control the disease?
Patients who have lost vision progressively due to glaucoma will be under great psychological stress, and caring to the needs of the patient may be challenging both to the doctor and family members. The family can help in multiple ways:
After a proper assessment by an eye-care professional, specially qualified in providing low vision services the following aids can be advised to the patient: